Supercharge your Credentialing
Get credentialed right the first time with our automated workflows and white glove service.
Book Demo
Provider Self-Service Portal

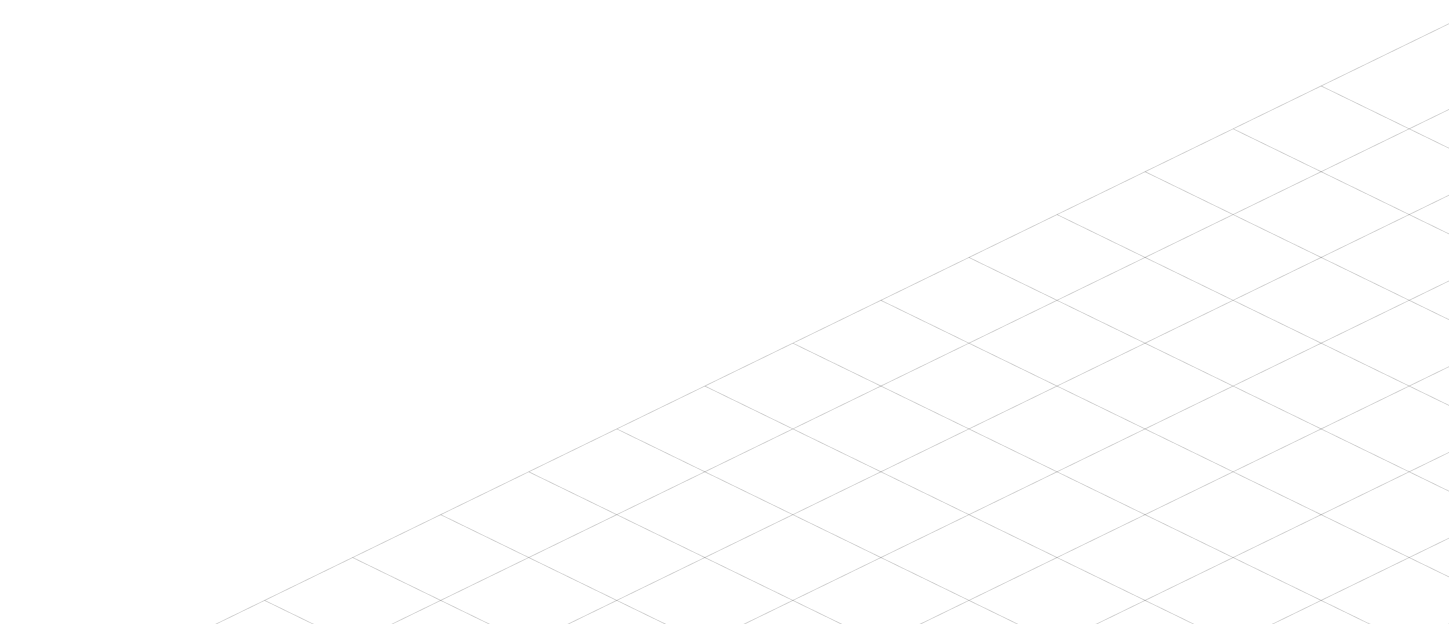
Built-In Monitoring

Automated Primary Source Verification

Payer Enrollment Support
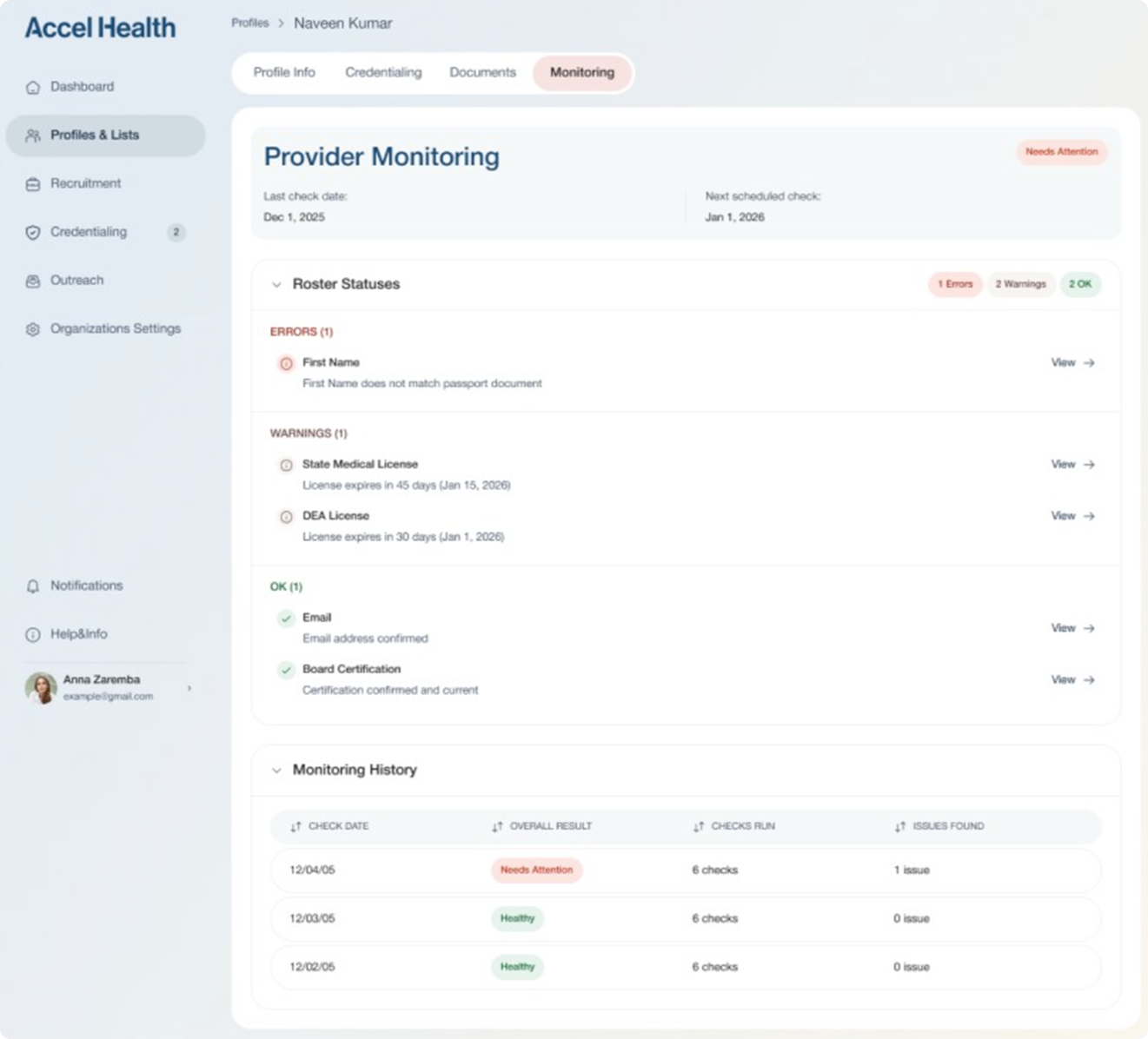
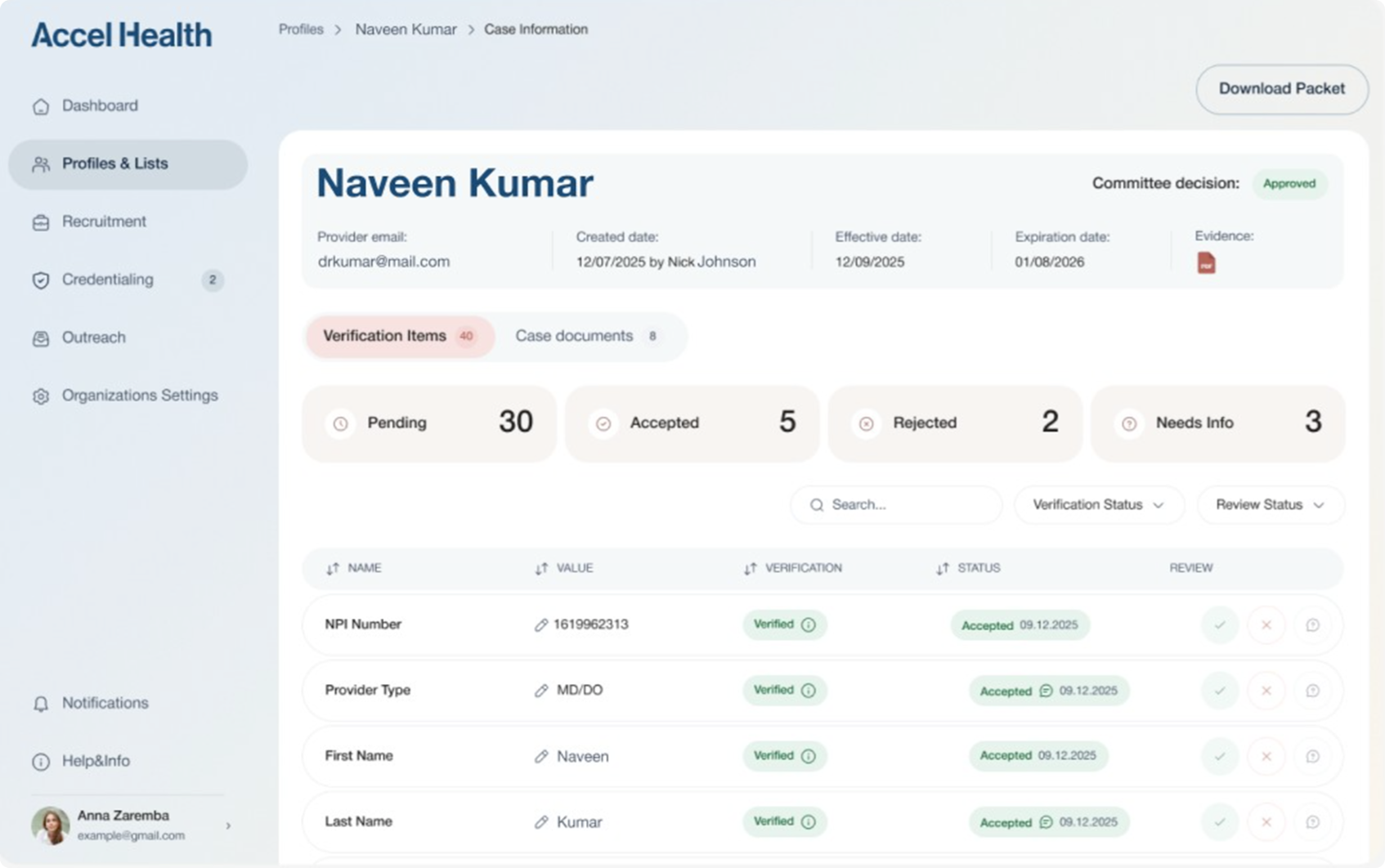
Complete Credentialing from start to finish
Accel Health handles the entire credentialing lifecycle from initial intake through payer enrollment. Automated PSV verifies credentials with primary sources. No spreadsheets, no manual tracking, no missed expirations.
Chat with our team
Built by credentialing experts
Accel Health was designed by credentialing professionals who understand what payers and committees actually require. Our workflows enforce completeness and accuracy at every step, resulting in significantly lower rejection rates. Get applications right the first time, every time!
Ready to credential 10x faster? Get early access.
Schedule a demo to get a sneak peek of how it works

